By Julia Simpson
One year into the COVID-19 pandemic, members of my extended family began reaching out to me with questions about the Pfizer-BioNTech and Moderna vaccines that the FDA had approved under Emergency Use Authorization (EUA) just a month prior1, 2. Anti-vaccine rhetoric rang through their social circles and media, and they hoped that, as a scientist, I could help answer some of their questions. I was thrilled to talk about the vaccines, honored that my family members were seeking my thoughts – but also filled with a self-imposed pressure about how the conversations would go. What if they asked a scientific question I didn’t know how to answer? What parts of the anti-vaccine rhetoric were resonating with them? What would be the most effective way for me to communicate?
Although these vaccines and others have since been granted full approval3, 4 and have been available to the American public for over a year, only 64.4% of Americans have been fully vaccinated against COVID-195. While this percentage rises to 75.9% when including those who have received at least one dose, these data indicate the existence of a clear group who has yet to be fully vaccinated. Continuing to be unvaccinated is not without consequence. In the past year, the Pennsylvania Department of Health has recorded6 that 85% of hospitalizations “with COVID-19 as the primary diagnosis/cause of admission were in unvaccinated, not fully vaccinated, or unknown vaccination status individuals.” This presents a chillingly clear illustration that, although a majority of individuals may be vaccinated, COVID-19 remains more dangerous for the unvaccinated minority.
When my family members reached out to me, I immediately agreed to the discussion for one overwhelming reason: because I love them, and I wanted more than anything for them to remain healthy and safe. My goal for this article is to provide a foundation of factual information as well as personal experience in talking about the vaccines to help you navigate COVID-19 conversations with vaccine-hesitant people in your life.
- Starting the conversation
In my experiences, conversations with vaccine-hesitant friends and family began when they reached out to me, not the other way around. This may not always be the case: maybe someone close to you has chosen not to get vaccinated and you’d like to talk with them about that choice, even though they have not reached out to you. If having this conversation is important to you, take care with how you approach it. For example, you can broach the topic with something like, “I understand that this may be a sensitive topic, but I know you haven’t yet gotten vaccinated against COVID-19. Is there any chance we could talk about that?” You could also say something along the lines of, “Would you mind walking me through what some of your hesitations are?” The essential thing to remember is that they might say no. If they do, you need to assess whether it would help or hinder your goals to push further, circle back to the topic another time, or let it go for the foreseeable future. As much as this may feel like an important conversation for you, it cannot be productive unless the other person is receptive to hear what you may have to say.
- Preparation
There were two elements that helped me understand what kind of conversations unvaccinated individuals who reached out to me were looking for:
A) they expressed interest in getting vaccinated, but didn’t feel quite ready to make the decision
B) they had been exposed to misinformation that raised fears and doubts.
Specific questions they had, which I found helpful to hone in on, included:
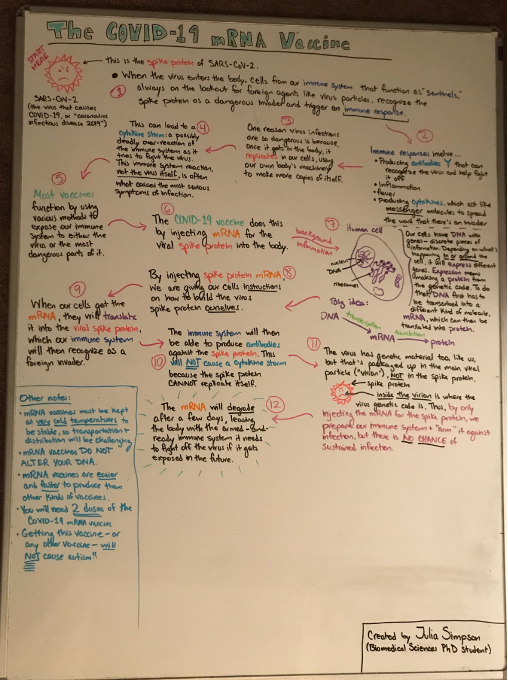
- How do mRNA vaccines work? Will the vaccine alter the recipient’s DNA?
- How can I trust the safety of this vaccine, given that it was developed so quickly?
- Why should I trust the vaccine, when we don’t know what’s in it? (We do, in fact, know what’s in the vaccines; all the components are published on the vaccine manufacturer’s websites)
- Is it safe to get the vaccine, even though we don’t know what the long-term effects might be?
- Isn’t the flu more dangerous than COVID-19? If so, why is it so important for me to get this vaccine?
An essential piece of the preparation process is understanding what someone’s concerns are, and why they have them. The above questions are reasonable and natural to ask. Once you understand the what and the why, the next step is research. It is extremely important that you obtain your background information from reliable sources7. Some examples of reliable sources are scientific journals, state health departments, governmental and international public health organizations, and vaccine manufacturers. While social media platforms and news outlets can certainly be stepping stones for you as you track down information, I would caution against citing them during your conversations with the vaccine-hesitant, as many news organizations are politically biased. That’s not to say that news sources can’t be helpful to you personally – several have written pieces on how to approach vaccination conversations with the vaccine-hesitant, which can be useful. However, base your conversations in the scientific literature. In summary: prior to the conversation, ask what questions the other person has; then, do your best to understand their hesitation and prepare your background information accordingly.
- The Talk
After having several of these conversations myself, and reading dozens of articles giving advice on how to successfully navigate them, the points and strategies I found most helpful are as follows. First: enter into the conversation with optimism, not anger – you both agreed to have this discussion, after all. One communications researcher emphasizes8 the importance of tone, stressing that “condescension, dismissiveness, and anger can completely shut down a conversation, and put people on the defensive.” In its official guidance on discussing vaccines with family and friends, the CDC urges9 the need to “acknowledge their emotions so they know they have been heard.” By acknowledging the other person’s concerns earnestly and respectfully, you can build trust. Striking this kind of tone from the beginning lays the foundation for a productive conversation.
As the discussion progresses, the next most important thing to do is be an active listener. Yes, you may have prepared a gorgeous, thorough set of statistics that, to you, state in crystal clear terms the importance of getting vaccinated against COVID-19; however, “pelting vaccine holdouts with facts and figures is all but certain to be a losing strategy10.” Why? Because, quite simply, “not everyone connects readily with facts and figures… so including the emotional appeal and personal experience is important8.” If the other person doesn’t respond to statistics, an active listener recognizes the lack of engagement and can switch tactics. Sharing anecdotal tales of the difficulties of COVID-19 symptoms may make the dangers of the virus more personal to the vaccine-hesitant individual11. Overall, active listening mainly involves being fully present in the conversation, acknowledging the other person’s concerns, and being adaptable as the discussion ebbs and flows.
The final critical step of COVID-19 vaccine conversations is to focus on your relationship with the other person, and emphasize that the reason you’re discussing this with them is because you care about them and value their presence in your life10. As one vaccine communication researcher puts it, “You have to keep saying over and over again how much the person means to you10.” When I spoke with family members about this topic, I made sure to make these sentiments clear throughout the talks. No matter how the conversation plays out, ending it with a reminder that all your information, statistics, advice, and anecdotes are being shared with the person because you care deeply for their health and well-being is a clear way to reiterate that you are happy that they were willing to engage in discussion, and that you are open to talk with them further about these subjects.
The COVID-19 Public Education Campaign encourages12 us to “listen and respond with empathy.” Empathy: the ability to understand and share the feelings of another13. It’s a nice, succinct phrase that is certainly a good starting point. If someone you know has yet to get vaccinated against COVID-19, and that’s a subject you’d like to discuss with them, I hope you find this article and the below resources helpful.
Compilation of Reliable Resources on COVID-19 Vaccines
TL:DR
Talking about vaccines with vaccine-hesitant friends and family can be difficult, but here are tips for a dynamic and empathetic conversation
References
- https://www.fda.gov/news-events/press-announcements/fda-takes-key-action-fight-against-covid-19-issuing-emergency-use-authorization-first-covid-19?utm_medium=email&utm_source=govdelivery
- https://www.fda.gov/news-events/press-announcements/fda-takes-additional-action-fight-against-covid-19-issuing-emergency-use-authorization-second-covid
- https://www.fda.gov/news-events/press-announcements/fda-approves-first-covid-19-vaccine
- https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-takes-key-action-approving-second-covid-19-vaccine
- https://www.mayoclinic.org/coronavirus-covid-19/vaccine-tracker
- https://www.health.pa.gov/topics/disease/coronavirus/Pages/Post-Vaccination-Data.aspx
- https://www.cosmopolitan.com/health-fitness/a37285088/how-to-talk-to-vaccine-skeptic-family-friends/
- https://www.popsci.com/health/how-talk-vaccine-hestitant-friends-family/
- https://www.cdc.gov/coronavirus/2019-ncov/vaccines/talk-about-vaccines.html
- https://www.washingtonpost.com/health/2021/07/24/how-talk-vaccine-hesitant-friends-family-about-getting-shot/
- https://www.apa.org/monitor/2021/03/covid-19-vaccines
- https://wecandothis.hhs.gov/resource/how-talk-about-covid-19-vaccines-friends-and-family
- https://www.merriam-webster.com/dictionary/empathy